
5 ways to get unstuck
We all have times in our lives when we feel stuck in a rut. We’re going through the same motions, each day, without actually getting wherever it is that we want to be. As a mental health coach, it’s part of my job to help people understand what changes they want to make, identify any potential obstacles, and begin to take steps towards what they want.

6 ways to cultivate a calm home
There are so many things happening in the world that are out of our control, and that can feel quite stressful and overwhelming for most of us. So in times of uncertainty, it can help to focus on areas of our life where we can bring in more calm and tranquility — like our home environment.

How to actually feel your feelings
As a therapist, it’s my job to help my clients learn to notice and tend to their biggest, most challenging feelings. So, let’s talk through how you can begin to make healthy, loving space for your feelings too.
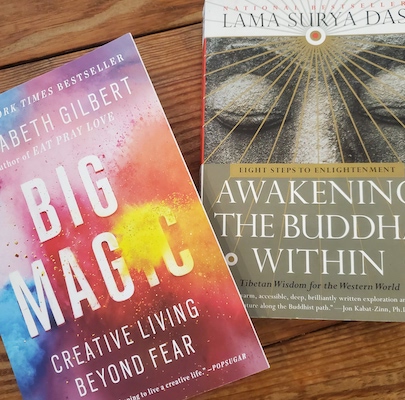
Our coaches’ favorite feel-good books
If you’re like us, curling up with a riveting book on a winter day is one of the best antidotes to the winter “mehs.” So, we went straight to our mental health coaches to ask what feel-good books they both love and recommend and we’re sharing all the highlights with you.

How to (finally) stop comparing yourself to others
How do we drop the comparisons and begin to focus on fully loving ourselves for who we are, not who we think we should be? There’s no miracle mantra that can snap us out of it, but as mental health coaches, we’ve learned tried and true steps that you can take to help you begin to drop the comparisons and develop true self-love.

7 ways to help kids manage stress
We can’t always protect our children from hard things, but we can help them develop healthy coping skills. Since it’s easier said than done, we’re here to support you with a few tried and true tips.

Your guide to creating healing art
Art has the power to connect, inspire, and heal us. Not only does creating our very own art allow for meaningful self-expression, but studies show that it can also help in treating depression, anxiety, and post-traumatic stress disorder. Read on for how to give your mental health a creative boost.

5 self-care myths… and how to get it right
While self-care is unique to everyone, it can help to start with identifying what self-care is and what it isn’t. So, I’ve decided to myth-bust all things surrounding self-care so that you can bring a little bit of it into your messiest, most imperfect days.